1- Clinical Research Development Unit (CRDU), Sayyad Shirazi Hospital, Golestan University of Medical Sciences, Gorgan, Iran
2- Department of Hemodialysis, 5th Azar Hospital, Golestan University of Medical Sciences, Gorgan, Iran
3- Metabolic Disorders Research Center, Golestan University of Medical Sciences, Golestan, Iran
4- Clinical Research Development Unit (CRDU), Sayyad Shirazi Hospital, Golestan University of Medical Sciences, Gorgan, Iran ,drsam74ir@ymail.com
2- Department of Hemodialysis, 5th Azar Hospital, Golestan University of Medical Sciences, Gorgan, Iran
3- Metabolic Disorders Research Center, Golestan University of Medical Sciences, Golestan, Iran
4- Clinical Research Development Unit (CRDU), Sayyad Shirazi Hospital, Golestan University of Medical Sciences, Gorgan, Iran ,
Full-Text [PDF 553 kb]
(519 Downloads)
| Abstract (HTML) (2158 Views)
Full-Text: (278 Views)
Introduction
The World Health Organization (WHO) officially declared COVID-19 a global pandemic in mid-June 2020 (1). Symptoms associated with COVID-19 are nonspecific, including fever (44-98% of patients), dry cough (68-76% of patients), and muscle pain (Observed in 18% of patients). Mortality rates vary, ranging from 2.3% in China to 7.2% in Italy (2,3).
In individuals affected by COVID-19, particular consideration should be given to certain demographic groups. Epidemiological investigations indicate that individuals with diabetes, hypertension, cardiovascular diseases, or those in the elderly demographic face an elevated susceptibility to contracting COVID-19, with a heightened likelihood of experiencing severe manifestations and requiring specialized care or succumbing to the disease (4,5). Patients undergoing maintenance dialysis are prone to an elevated risk of contracting COVID-19 and experiencing its complications (3). Epidemiological studies indicate that the kidney is an important target of COVID-19 (6). Acute kidney injury (AKI) occurs in 5-15% of cases, and the presence of COVID-19 is identified as an independent risk factor for mortality (7). Patients with Chronic Kidney Disease (CKD), those undergoing chronic replacement therapy, and kidney transplant recipients are also affected by COVID-19. Hemodialysis patients may have a higher risk of contracting COVID-19 because of possible cross-contamination in confined spaces and issues with both their adaptive and innate immune systems. Furthermore, the hemodialysis patient population exhibits a higher prevalence of severe comorbidities such as cardiovascular disease, hypertension, and diabetes mellitus, all of which are linked to an elevated risk of adverse outcomes. This review is centered on exploring the clinical aspects of COVID-19 in hemodialysis patients (8).
After the binding of the SARS-CoV-2 antigen protein to angiotensin-converting enzyme 2 (ACE2) receptors, the S protein undergoes cleavage and activation by the serum family of membrane proteases (TMPRSS). This activation enables the virus to cleave the fusion peptide, facilitating its release (9). Acute kidney failure in COVID-19 may result from a synergistic effect involving both the direct cytotoxic impact of the virus and the systemic inflammatory response triggered by cytokines. This form of renal failure is particularly evident in critically ill patients, those with acute respiratory distress syndrome (ARDS), and individuals requiring intensive care unit (ICU) admission. Additional potential mechanisms contributing to acute renal failure include acute tubular necrosis (ATN) due to multiple organ failure and shock, as well as a potential pre-renal cause stemming from volume depletion associated with reduced oral intake and high fever. Factors such as drug toxicity, hemodynamic involvement, and exposure to contrast material also have the potential to play a role in this context (10).
Evaluation for acute kidney failure in COVID-19 should follow the same protocols used for other causes of acute kidney failure. Several factors can contribute to acute renal failure, including acute ischemic tubular injury, nephrotoxic acute tubular injury, or a combination of both, acute interstitial nephritis, glomerular disease, prerenal azotemia, and unspecified causes. Some factors involved in these various conditions may include hypotension, shock, atrial fibrillation, prolonged volume depletion, rhabdomyolysis, exposure to toxic agents such as vancomycin and iodinated contrast, as well as evident proteinuria (11). Additionally, the degree and severity of lung involvement can be evaluated with CT intensity score. This quantification plays an important role in modifying the treatment plan in some cases in critical patients with COVID-19. The CT severity score reveals the actual lung involvement percentage due to the COVID-19. Briefly, CT severity score ≤ 8 indicates mild disease, CT severity score between 9 -15 means moderate disease, and CT severity score >15 reveals severe disease (12). Further, hemodialysis patients may be susceptible to COVID-19 and its systemic consequences due to the following reasons: 1. increased risk of transmission, 2. chronic immune system dysfunction, 3. endothelial dysfunction, 4. organ damage with reduced structural or functional reserve, and 5. prior comorbidity and increased risk of renal system dysfunction due to reduced structural organ reserve (3,10).
The effect of the COVID-19 epidemic on chronic kidney disease and end-stage kidney patients has not yet been fully determined. Considering the low immune function of uremic patients, the situation of the epidemic of COVID-19 in these patients should not be ignored. In this study, we intend to describe the frequency of COVID-19 and its characteristics in the main hemodialysis centers of the Golestan Province. In this study, the epidemiological, clinical, laboratory, and radiological characteristics of these patients are investigated, and we expect that our findings will contribute to the proper management of this disease in dialysis units.
Methods
This descriptive cross-sectional study was conducted on patients undergoing maintenance hemodialysis with positive RT-PCR (Real-Time PCR) and chest CT (Computed Tomography) scan graph for COVID-19 in the hemodialysis department of 5 Azar and Sayad Shirazi Hospital in Golestan Province in 2019. After obtaining the relevant ethical permits from the academic authorities and coordinating with the officials of 5 Azar and Sayyad Shirazi Hospital to access and use the information of hospitalization records of the dialysis patients infected with COVID-19 in those centers, the required information was obtained through the patients' files.
Demographic information of patients (Age, gender, ethnicity), clinical symptoms of patients (Fever, myalgia, shortness of breath, dry cough, anorexia, weakness, and lethargy, decreased level of consciousness) and laboratory tests ((Calcium, phosphorus), sodium, potassium, CBC (Complete Blood Count), AlP (Alkaline Phosphatase), TG (Triglycerides), Chol (Cholesterol), AST (Aspartate Transferase), ALT (Alanine Transferase), Alb (Albumin), Ferritin, CRP (C-Reactive Protein) and ESR (Erythrocyte Sedimentation Rate)), patient dialysis variables (Dialysis adequacy (KT/V), time per session in hours, number of sessions per week) and The radiological data (CT scan of the chest) were recorded by the operator in the Registration form. Dialysis adequacy usually refers to how well toxins and waste products are removed from the patient's blood, which has a major impact on their well-being. Moreover, Kt/V is a metric used to assess the effectiveness of a hemodialysis session.
Also, additionally, information regarding the underlying diseases of the patients was collected. During the follow-up period, the cases of death of these patients were recorded, and the possible cause of death was suggested by the research team, based on its time, place and, clinical manifestations.
Research limitations
Access to a sufficient and appropriate number of patient samples was one of the study's limitations. Another limitation of this study is the lack of follow-up on discharged patients and the lack of measuring their mortality rates over the medium to long term. Besides, due to the high cost of inflammatory markers kits, we could not examine all of these markers in all of the patients.
Ethical consideration
This study, conducted on hemodialysis patients with COVID-19, prioritized ethical standards. Necessary permits were obtained, and collaboration with hospital officials ensured confidential use of patients’ records. Patient confidentiality was strictly maintained, and informed consent was obtained when applicable. Transparency and communication were upheld to safeguard participant welfare and research integrity. The study adhered to ethical guidelines in all stages, respecting patient rights and promoting data security.
Statistical analysis
All results were analyzed using SPSS 21.0 (SPSS, Inc., Chicago, IL, USA). To determine the normality, we performed the Shapiro-Wilk test. For data analysis, we used the student T-test or Mann-Whitney U test according to the normality results. Moreover, p <0.05 was considered to indicate a statistically significant difference. In addition, we considered the conditions of the Chi-square test such as Random Sampling, as well each observation is related to one person, and no person is counted twice in the sampling.
Results
Demographic frequency of hemodialysis patients with COVID-19
Out of 198 hemodialysis patients, 30 qualified for this study. Thirty-five patients were excluded because they had missing or negative PCR results, did not require hospitalization, or had passed away. The mean age of the cohort was 58.97 ± 11.88 years (Range 34-83). Of these, 16 (53.3%) were female and 14 (46.7%) males The majority of the patients identified as Persian (26 patients, 86.7%), with smaller numbers representing Turkman (1 patient, 3.3%), Sistani (2 patients, 6.7%), and Cossack (1 patient, 3.3%) ethnicities. The distribution of body mass index (BMI) showed that 17 patients (56.6%) had a BMI within the 18.5-24.9 range, seven patients (23.3%) were considered overweight with a BMI of 25-29.9, and six patients (20%) were classified as obese with a BMI of 30-34.9. None of the patients had a BMI below 18.5 or 35 or above.
Proportion of underlying disease history with COVID-19
This study analyzed the medical records of hemodialysis patients with COVID-19 and found that hypertension was the most common comorbidity, affecting 24 patients (76.7%), followed by diabetes, which was present in 15 patients (50%). Coronary heart disease was observed in 3 patients (10%), and one patient (3.3%) had a history of kidney transplantation. The initial clinical symptoms primarily consisted of fever (80%), dyspnea (83.3%), weakness and lethargy (63.3%), and anorexia (33.3%). Notably, cough and myalgia were reported in 10% and 33.3% of patients, respectively. COVID-19 diagnosis was confirmed through PCR testing. Radiological evaluation showed ground-glass opacities in 46.7% of cases, linear opacities in 26.7%, and bilateral consolidation in 16.7%, with multilobar involvement noted in 10% of patients. In the short term, 26 patients (86.6%) were discharged, and 4 patients (13.4%) passed away during the study period.
Laboratory findings in hemodialysis patients with COVID-19
Mann-Whitney U tests revealed that age, white blood cell (WBC) count, and serum creatinine levels were significant predictors of mortality (p < 0.05), with deceased patients being older and having higher values in these parameters. No significant difference in body mass index (BMI) was found between survivors and non-survivors. The Kolmogorov-Smirnov test confirmed the normality of other laboratory variables, including triglycerides, cholesterol, platelets, lactate dehydrogenase (LDH), blood urea nitrogen (BUN), ferritin, calcium, potassium, and phosphorus (p > 0.05), allowing for comparison using Student’s t-test. As shown in Table 1, none of these variables differed significantly between the two groups (p > 0.05), except for age (p = 0.02), WBC count (p = 0.037), and creatinine (p = 0.033).
Association of comorbidities with mortality of hemodialysis patients with COVID-19
Exact fisher test analysis indicated that COVID-19 patients with a history of diabetes had significantly higher mortality rates (P-Value < 0.05). However, no significant associations were found between mortality and conditions such as coronary heart disease, polycystic kidney disease, or prior kidney transplantation (P-Value > 0.05). As summarized in Table 2, these results emphasize diabetes as critical comorbidities associated with increased mortality in this group.
Association of severe symptoms with mortality of hemodialysis patients with COVID-19
The results from the exact Fisher test indicated that patients with cough complaints (P-Value = 0.128) and malaise (P-Value = 0.485) did not have a significant association with a higher mortality rate in ESRD patients with COVID-19. Additionally, the exact Fisher test showed that other severe symptoms were not associated with the COVID-19 mortality rate in ESRD patients. These findings are summarized in Table 3.
Correlation of CRP serum levels with hemodialysis duration in hemodialysis patients with COVID-19
In this study, our findings revealed that the serum CRP levels did not correlate with hemodialysis duration (R = 0.267, P-Value = 0.154). In contrast, the obtained results from Spearman’s correlation revealed the serum CRP levels had a significant negative correlation with ESRD in hemodialysis patients with COVID-19 (R = 0.527, P-Value < 0.003). Additionally, the results from Spearman’s correlation indicated that the hemodialysis duration, PCR results, and CRP serum levels had no significant correlation with any type of pulmonary involvement in ESRD patients with COVID-19, which is diagnosed by chest CT graph (P-Value > 0.05).
Hemodialysis patients with COVID-19 outcomes
The CT scan results highlighted a significant difference between recovered and deceased ESRD patients with COVID-19. These findings are presented in Table 4.
Discussion
This research aims to describe the clinical attributes and immediate repercussions experienced by a cohort of 30 chronic hemodialysis patients afflicted with COVID-19 in Gorgan province in 2019. The mean age of the participants stood at 58.97±11.88 years, signaling an elder populace in comparison to broader investigations encompassing hemodialysis patients, typically ranging between 57 and 66 years of age (3).
The clinical outcomes of this study show that the majority of hemodialysis patients with COVID-19 were discharged (86.6%), indicating effective acute management for most patients. However, the observed mortality rate of 13.4% highlights the significant impact of COVID-19 on this population. Bahat et al. reported a mortality rate of 20% among hemodialysis patients with COVID-19, with other studies indicating rates of 16% and 28% in groups of 37 and 25 hemodialysis patients, respectively (3,13). These rates were notably higher than the mortality rates observed in the general population, ranging from 0.8% to 1.4% (14-16). The elevated mortality in hemodialysis patients can be attributed to various factors, including concurrent diseases, chronic kidney failure, and immunosuppression induced by high uremia (17).
The clinical outcomes of this study indicate that the majority of hemodialysis patients with COVID-19 were discharged (86.6%), which indicates the effective acute management for most patients. However, the observed mortality rate of 13.4% underscores the severe impact of COVID-19 on this population. The increased susceptibility of men to the infection may be attributed to increased levels of ACE receptors, particularly in podocyte cells and proximal convoluted tubule cells that express the ACE2 and TMPRSS genes, which are the main targets of the SARS-CoV-2 virus. It is notable that kidney tissue exhibits greater ACE2 gene expression than lung tissue, with the binding affinity of SARS-CoV-2 receptors to ACE2 being 10 to 20 times higher than that of SARS-CoV-1 (9,17-19). Bwire et al. suggested that males were more susceptible to SARS-CoV-2 infection due to higher ACE2 receptor expression levels (20). Chai et al. (21) and Bwire et al. (20) provided evidence of increased ACE2 expression in male kidney tissues compared to females’ kidney tissues, potentially contributing to the gender disparity in infection rates.
The strong association between diabetes and increased mortality emphasizes the critical need for effective management of these comorbidities to enhance clinical outcomes. Additionally, radiological abnormalities and the presence of ESRD are significant predictors of prognosis, highlighting the necessity for close monitoring and, when appropriate, more intensive therapeutic interventions. Xiong et al. (17) 95.4% of patients had at least one comorbidity, with cardiovascular disease associated with hypertension and diabetes being the most prevalent. Fisher et al. supported these findings and identified diabetes, hypertension, coronary artery disease, and pulmonary disease as the most common comorbidities among hemodialysis patients with COVID-19 (22). Li et al.’s study highlighted the predominance of high blood pressure and diabetes in ESRD patients with COVID-19. Furthermore, Li et al. emphasized the significance of respiratory diseases as additional common comorbidities in this patient population during the COVID-19 pandemic (23).
Clinical symptoms show a high incidence of fever (80%) and dyspnea (83.3%), indicating a severe COVID-19 disease course in hemodialysis patients. Radiological findings, particularly ground-glass opacities and bilateral consolidations, further emphasize the significant pulmonary involvement in this vulnerable group. Our findings are in the same direction as Valeri et al., Fisher et al., and Xiong et al., where fever consistently emerged as the primary clinical symptom, followed by cough, fatigue, and shortness of breath in patients with COVID-19 (17,18,22). Adwan et al. corroborated these clinical observations, highlighting fever, respiratory distress, and fatigue as the most prevalent symptoms among hemodialysis patients with COVID-19 (24). On the other hand, Valeri et al. found one-sided opacity in 10% of patients in chest radiographs, with over half of the recovered patients showing multiple or one-sided infiltrations (18). Goicoechea and Ma reported a ground glass radiological appearance with bilateral and peripheral patterns in 85.7% and 64% of patients, respectively (25,26).
In our study, comparison of clinical and laboratory parameters between discharged and deceased hemodialysis patients with COVID-19 demonstrated that non-survivors were generally older and exhibited elevated white blood cell counts and serum creatinine levels relative to recovered patients. Other laboratory values showed no significant differences between groups. Comorbidities such as diabetes were more common among the deceased patients, and their clinical presentation, including symptoms like weakness and lethargy, differed significantly from survivors (27). These findings are consistent with the research by Zhou et al. (2020), which reported higher mortality rates associated with comorbid conditions prevalent in hemodialysis patients, thus validating our results (28).
Laboratory analyses revealed that elevated white blood cell counts and serum creatinine levels were significant prognostic indicators associated with mortality. The absence of notable differences in other laboratory parameters underscores the need for further research to identify additional predictive biomarkers. In Valeri et al.’s study, a 14-day follow-up showed that 18 patients (31%) died within six days of hospital admission. Deceased patients had significantly higher baseline levels of white blood cells, lactate dehydrogenase (LDH), and C-reactive protein (CRP) compared to survivors (P-Value = 0.04) (18). Ma et al. involving 230 hemodialysis patients in Wuhan, China, 15 individuals (6.25%) died from COVID-19, with cardiovascular disease, cerebrovascular disease, and hyperkalemia identified as leading causes of death (29). Laboratory findings reveal that elevated WBC counts and creatinine levels serve as significant prognostic markers associated with mortality (19). Findings from Valeri's, Yiqiong et al.’s, and Fisher’s studies further support the adverse prognostic indicators identified in our research, including elevated inflammatory markers and underlying cardiovascular conditions.
This study showed a significant relationship between some demographic factors, comorbidities, symptoms, and laboratory findings with patient outcomes. For example, increased WBC count and creatinine level were identified as important prognostic markers associated with mortality. In addition, comorbidities such as diabetes were strongly associated with increased mortality rates. These findings emphasize the importance of comprehensive patient assessment and appropriate treatment strategies to optimize outcomes in this vulnerable population.
Despite the lack of long-term follow-up data, this study provides valuable insights into the acute effects of COVID-19 on hemodialysis patients. Future research should include long-term follow-up to assess ongoing outcomes and potential complications. Additionally, larger, multicenter studies are needed to validate these findings and explore further factors influencing outcomes in this vulnerable population. Enhanced preventive measures, early interventions, and regular monitoring using CT scans and laboratory markers are crucial for managing hemodialysis patients with COVID-19.
Conclusion
In summary, this study highlights the clinical outcomes of hemodialysis patients with COVID-19. While most patients were discharged, a notable mortality rate underscores the severity of the disease. Common symptoms and significant radiological findings emphasize the acute presentation of COVID-19 in this population. Laboratory markers, especially elevated WBC counts and creatinine levels, serve as important prognostic indicators. Management of comorbid conditions like diabetes is crucial, and the study underscores the need for vigilant monitoring and potentially more aggressive treatment strategies. Further research is warranted to validate these findings and explore additional factors affecting outcomes in hemodialysis patients with COVID-19.
Acknowledgement
The authors thank the research committee of Golestan University of Medical Sciences and also this work was supported by the research committee of Golestan University of Medical Sciences.
Funding sources
This work was supported by the Research Committee of Golestan University of Medical Sciences with the grant number IR.GOUMS.REC.1399.377.
Ethical statement
Ethical approval was obtained from the Golestan University research committee, under approval number IR.GOUMS.REC.1399.377. Written informed consent was obtained from all patients or their legal guardians before their inclusion in the study. All patient data were anonymized to ensure privacy and confidentiality.
Conflicts of interest
The authors have no financial or proprietary interests in any material discussed in this article.
Author contributions
The role of each participant is as follows: SA and MM conceived this study and were the supervisors. SJ, and AR. collected and analyzed the data. Also, ZM and AR. drafted the manuscript. All authors read and approved the final version of the manuscript.
The World Health Organization (WHO) officially declared COVID-19 a global pandemic in mid-June 2020 (1). Symptoms associated with COVID-19 are nonspecific, including fever (44-98% of patients), dry cough (68-76% of patients), and muscle pain (Observed in 18% of patients). Mortality rates vary, ranging from 2.3% in China to 7.2% in Italy (2,3).
In individuals affected by COVID-19, particular consideration should be given to certain demographic groups. Epidemiological investigations indicate that individuals with diabetes, hypertension, cardiovascular diseases, or those in the elderly demographic face an elevated susceptibility to contracting COVID-19, with a heightened likelihood of experiencing severe manifestations and requiring specialized care or succumbing to the disease (4,5). Patients undergoing maintenance dialysis are prone to an elevated risk of contracting COVID-19 and experiencing its complications (3). Epidemiological studies indicate that the kidney is an important target of COVID-19 (6). Acute kidney injury (AKI) occurs in 5-15% of cases, and the presence of COVID-19 is identified as an independent risk factor for mortality (7). Patients with Chronic Kidney Disease (CKD), those undergoing chronic replacement therapy, and kidney transplant recipients are also affected by COVID-19. Hemodialysis patients may have a higher risk of contracting COVID-19 because of possible cross-contamination in confined spaces and issues with both their adaptive and innate immune systems. Furthermore, the hemodialysis patient population exhibits a higher prevalence of severe comorbidities such as cardiovascular disease, hypertension, and diabetes mellitus, all of which are linked to an elevated risk of adverse outcomes. This review is centered on exploring the clinical aspects of COVID-19 in hemodialysis patients (8).
After the binding of the SARS-CoV-2 antigen protein to angiotensin-converting enzyme 2 (ACE2) receptors, the S protein undergoes cleavage and activation by the serum family of membrane proteases (TMPRSS). This activation enables the virus to cleave the fusion peptide, facilitating its release (9). Acute kidney failure in COVID-19 may result from a synergistic effect involving both the direct cytotoxic impact of the virus and the systemic inflammatory response triggered by cytokines. This form of renal failure is particularly evident in critically ill patients, those with acute respiratory distress syndrome (ARDS), and individuals requiring intensive care unit (ICU) admission. Additional potential mechanisms contributing to acute renal failure include acute tubular necrosis (ATN) due to multiple organ failure and shock, as well as a potential pre-renal cause stemming from volume depletion associated with reduced oral intake and high fever. Factors such as drug toxicity, hemodynamic involvement, and exposure to contrast material also have the potential to play a role in this context (10).
Evaluation for acute kidney failure in COVID-19 should follow the same protocols used for other causes of acute kidney failure. Several factors can contribute to acute renal failure, including acute ischemic tubular injury, nephrotoxic acute tubular injury, or a combination of both, acute interstitial nephritis, glomerular disease, prerenal azotemia, and unspecified causes. Some factors involved in these various conditions may include hypotension, shock, atrial fibrillation, prolonged volume depletion, rhabdomyolysis, exposure to toxic agents such as vancomycin and iodinated contrast, as well as evident proteinuria (11). Additionally, the degree and severity of lung involvement can be evaluated with CT intensity score. This quantification plays an important role in modifying the treatment plan in some cases in critical patients with COVID-19. The CT severity score reveals the actual lung involvement percentage due to the COVID-19. Briefly, CT severity score ≤ 8 indicates mild disease, CT severity score between 9 -15 means moderate disease, and CT severity score >15 reveals severe disease (12). Further, hemodialysis patients may be susceptible to COVID-19 and its systemic consequences due to the following reasons: 1. increased risk of transmission, 2. chronic immune system dysfunction, 3. endothelial dysfunction, 4. organ damage with reduced structural or functional reserve, and 5. prior comorbidity and increased risk of renal system dysfunction due to reduced structural organ reserve (3,10).
The effect of the COVID-19 epidemic on chronic kidney disease and end-stage kidney patients has not yet been fully determined. Considering the low immune function of uremic patients, the situation of the epidemic of COVID-19 in these patients should not be ignored. In this study, we intend to describe the frequency of COVID-19 and its characteristics in the main hemodialysis centers of the Golestan Province. In this study, the epidemiological, clinical, laboratory, and radiological characteristics of these patients are investigated, and we expect that our findings will contribute to the proper management of this disease in dialysis units.
Methods
This descriptive cross-sectional study was conducted on patients undergoing maintenance hemodialysis with positive RT-PCR (Real-Time PCR) and chest CT (Computed Tomography) scan graph for COVID-19 in the hemodialysis department of 5 Azar and Sayad Shirazi Hospital in Golestan Province in 2019. After obtaining the relevant ethical permits from the academic authorities and coordinating with the officials of 5 Azar and Sayyad Shirazi Hospital to access and use the information of hospitalization records of the dialysis patients infected with COVID-19 in those centers, the required information was obtained through the patients' files.
Demographic information of patients (Age, gender, ethnicity), clinical symptoms of patients (Fever, myalgia, shortness of breath, dry cough, anorexia, weakness, and lethargy, decreased level of consciousness) and laboratory tests ((Calcium, phosphorus), sodium, potassium, CBC (Complete Blood Count), AlP (Alkaline Phosphatase), TG (Triglycerides), Chol (Cholesterol), AST (Aspartate Transferase), ALT (Alanine Transferase), Alb (Albumin), Ferritin, CRP (C-Reactive Protein) and ESR (Erythrocyte Sedimentation Rate)), patient dialysis variables (Dialysis adequacy (KT/V), time per session in hours, number of sessions per week) and The radiological data (CT scan of the chest) were recorded by the operator in the Registration form. Dialysis adequacy usually refers to how well toxins and waste products are removed from the patient's blood, which has a major impact on their well-being. Moreover, Kt/V is a metric used to assess the effectiveness of a hemodialysis session.
Also, additionally, information regarding the underlying diseases of the patients was collected. During the follow-up period, the cases of death of these patients were recorded, and the possible cause of death was suggested by the research team, based on its time, place and, clinical manifestations.
Research limitations
Access to a sufficient and appropriate number of patient samples was one of the study's limitations. Another limitation of this study is the lack of follow-up on discharged patients and the lack of measuring their mortality rates over the medium to long term. Besides, due to the high cost of inflammatory markers kits, we could not examine all of these markers in all of the patients.
Ethical consideration
This study, conducted on hemodialysis patients with COVID-19, prioritized ethical standards. Necessary permits were obtained, and collaboration with hospital officials ensured confidential use of patients’ records. Patient confidentiality was strictly maintained, and informed consent was obtained when applicable. Transparency and communication were upheld to safeguard participant welfare and research integrity. The study adhered to ethical guidelines in all stages, respecting patient rights and promoting data security.
Statistical analysis
All results were analyzed using SPSS 21.0 (SPSS, Inc., Chicago, IL, USA). To determine the normality, we performed the Shapiro-Wilk test. For data analysis, we used the student T-test or Mann-Whitney U test according to the normality results. Moreover, p <0.05 was considered to indicate a statistically significant difference. In addition, we considered the conditions of the Chi-square test such as Random Sampling, as well each observation is related to one person, and no person is counted twice in the sampling.
Results
Demographic frequency of hemodialysis patients with COVID-19
Out of 198 hemodialysis patients, 30 qualified for this study. Thirty-five patients were excluded because they had missing or negative PCR results, did not require hospitalization, or had passed away. The mean age of the cohort was 58.97 ± 11.88 years (Range 34-83). Of these, 16 (53.3%) were female and 14 (46.7%) males The majority of the patients identified as Persian (26 patients, 86.7%), with smaller numbers representing Turkman (1 patient, 3.3%), Sistani (2 patients, 6.7%), and Cossack (1 patient, 3.3%) ethnicities. The distribution of body mass index (BMI) showed that 17 patients (56.6%) had a BMI within the 18.5-24.9 range, seven patients (23.3%) were considered overweight with a BMI of 25-29.9, and six patients (20%) were classified as obese with a BMI of 30-34.9. None of the patients had a BMI below 18.5 or 35 or above.
Proportion of underlying disease history with COVID-19
This study analyzed the medical records of hemodialysis patients with COVID-19 and found that hypertension was the most common comorbidity, affecting 24 patients (76.7%), followed by diabetes, which was present in 15 patients (50%). Coronary heart disease was observed in 3 patients (10%), and one patient (3.3%) had a history of kidney transplantation. The initial clinical symptoms primarily consisted of fever (80%), dyspnea (83.3%), weakness and lethargy (63.3%), and anorexia (33.3%). Notably, cough and myalgia were reported in 10% and 33.3% of patients, respectively. COVID-19 diagnosis was confirmed through PCR testing. Radiological evaluation showed ground-glass opacities in 46.7% of cases, linear opacities in 26.7%, and bilateral consolidation in 16.7%, with multilobar involvement noted in 10% of patients. In the short term, 26 patients (86.6%) were discharged, and 4 patients (13.4%) passed away during the study period.
Laboratory findings in hemodialysis patients with COVID-19
Mann-Whitney U tests revealed that age, white blood cell (WBC) count, and serum creatinine levels were significant predictors of mortality (p < 0.05), with deceased patients being older and having higher values in these parameters. No significant difference in body mass index (BMI) was found between survivors and non-survivors. The Kolmogorov-Smirnov test confirmed the normality of other laboratory variables, including triglycerides, cholesterol, platelets, lactate dehydrogenase (LDH), blood urea nitrogen (BUN), ferritin, calcium, potassium, and phosphorus (p > 0.05), allowing for comparison using Student’s t-test. As shown in Table 1, none of these variables differed significantly between the two groups (p > 0.05), except for age (p = 0.02), WBC count (p = 0.037), and creatinine (p = 0.033).
|
Table 1. Mean and standard deviation of laboratory and demographic variables in hemodialysis patients with COVID-19
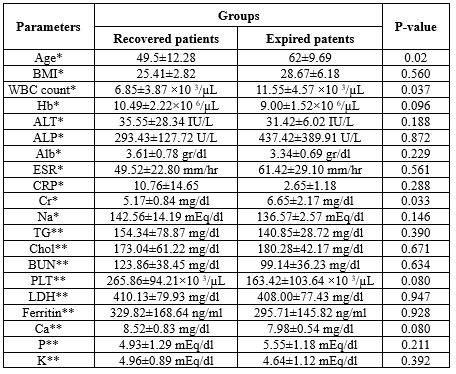 * Means Mann-Whitney U test and ** Means Student T-test. |
Exact fisher test analysis indicated that COVID-19 patients with a history of diabetes had significantly higher mortality rates (P-Value < 0.05). However, no significant associations were found between mortality and conditions such as coronary heart disease, polycystic kidney disease, or prior kidney transplantation (P-Value > 0.05). As summarized in Table 2, these results emphasize diabetes as critical comorbidities associated with increased mortality in this group.
|
Table 2. Frequency and percentage of the underlying disease of hemodialysis patients with COVID-19 based on the patient's outcome
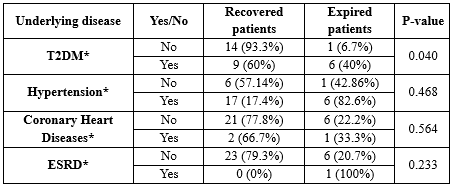 * Exact fisher test. |
The results from the exact Fisher test indicated that patients with cough complaints (P-Value = 0.128) and malaise (P-Value = 0.485) did not have a significant association with a higher mortality rate in ESRD patients with COVID-19. Additionally, the exact Fisher test showed that other severe symptoms were not associated with the COVID-19 mortality rate in ESRD patients. These findings are summarized in Table 3.
|
Table 3. Examining the frequency and percentage of initial complaints and clinical manifestations of patients with COVID-19 based on the patient's outcomes
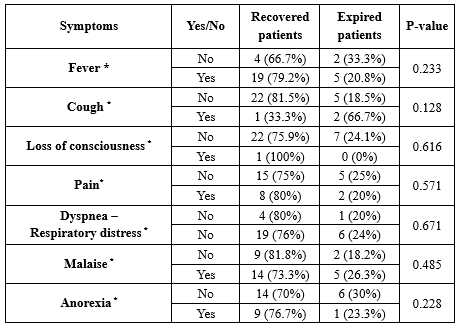 * Exact fisher test. |
In this study, our findings revealed that the serum CRP levels did not correlate with hemodialysis duration (R = 0.267, P-Value = 0.154). In contrast, the obtained results from Spearman’s correlation revealed the serum CRP levels had a significant negative correlation with ESRD in hemodialysis patients with COVID-19 (R = 0.527, P-Value < 0.003). Additionally, the results from Spearman’s correlation indicated that the hemodialysis duration, PCR results, and CRP serum levels had no significant correlation with any type of pulmonary involvement in ESRD patients with COVID-19, which is diagnosed by chest CT graph (P-Value > 0.05).
Hemodialysis patients with COVID-19 outcomes
The CT scan results highlighted a significant difference between recovered and deceased ESRD patients with COVID-19. These findings are presented in Table 4.
|
Table 4. Mean and standard deviation of mortality and recovery in hemodialysis patients with COVID-19
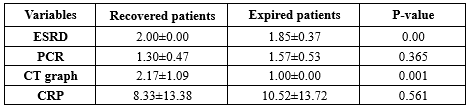 * Student T-test. |
Discussion
This research aims to describe the clinical attributes and immediate repercussions experienced by a cohort of 30 chronic hemodialysis patients afflicted with COVID-19 in Gorgan province in 2019. The mean age of the participants stood at 58.97±11.88 years, signaling an elder populace in comparison to broader investigations encompassing hemodialysis patients, typically ranging between 57 and 66 years of age (3).
The clinical outcomes of this study show that the majority of hemodialysis patients with COVID-19 were discharged (86.6%), indicating effective acute management for most patients. However, the observed mortality rate of 13.4% highlights the significant impact of COVID-19 on this population. Bahat et al. reported a mortality rate of 20% among hemodialysis patients with COVID-19, with other studies indicating rates of 16% and 28% in groups of 37 and 25 hemodialysis patients, respectively (3,13). These rates were notably higher than the mortality rates observed in the general population, ranging from 0.8% to 1.4% (14-16). The elevated mortality in hemodialysis patients can be attributed to various factors, including concurrent diseases, chronic kidney failure, and immunosuppression induced by high uremia (17).
The clinical outcomes of this study indicate that the majority of hemodialysis patients with COVID-19 were discharged (86.6%), which indicates the effective acute management for most patients. However, the observed mortality rate of 13.4% underscores the severe impact of COVID-19 on this population. The increased susceptibility of men to the infection may be attributed to increased levels of ACE receptors, particularly in podocyte cells and proximal convoluted tubule cells that express the ACE2 and TMPRSS genes, which are the main targets of the SARS-CoV-2 virus. It is notable that kidney tissue exhibits greater ACE2 gene expression than lung tissue, with the binding affinity of SARS-CoV-2 receptors to ACE2 being 10 to 20 times higher than that of SARS-CoV-1 (9,17-19). Bwire et al. suggested that males were more susceptible to SARS-CoV-2 infection due to higher ACE2 receptor expression levels (20). Chai et al. (21) and Bwire et al. (20) provided evidence of increased ACE2 expression in male kidney tissues compared to females’ kidney tissues, potentially contributing to the gender disparity in infection rates.
The strong association between diabetes and increased mortality emphasizes the critical need for effective management of these comorbidities to enhance clinical outcomes. Additionally, radiological abnormalities and the presence of ESRD are significant predictors of prognosis, highlighting the necessity for close monitoring and, when appropriate, more intensive therapeutic interventions. Xiong et al. (17) 95.4% of patients had at least one comorbidity, with cardiovascular disease associated with hypertension and diabetes being the most prevalent. Fisher et al. supported these findings and identified diabetes, hypertension, coronary artery disease, and pulmonary disease as the most common comorbidities among hemodialysis patients with COVID-19 (22). Li et al.’s study highlighted the predominance of high blood pressure and diabetes in ESRD patients with COVID-19. Furthermore, Li et al. emphasized the significance of respiratory diseases as additional common comorbidities in this patient population during the COVID-19 pandemic (23).
Clinical symptoms show a high incidence of fever (80%) and dyspnea (83.3%), indicating a severe COVID-19 disease course in hemodialysis patients. Radiological findings, particularly ground-glass opacities and bilateral consolidations, further emphasize the significant pulmonary involvement in this vulnerable group. Our findings are in the same direction as Valeri et al., Fisher et al., and Xiong et al., where fever consistently emerged as the primary clinical symptom, followed by cough, fatigue, and shortness of breath in patients with COVID-19 (17,18,22). Adwan et al. corroborated these clinical observations, highlighting fever, respiratory distress, and fatigue as the most prevalent symptoms among hemodialysis patients with COVID-19 (24). On the other hand, Valeri et al. found one-sided opacity in 10% of patients in chest radiographs, with over half of the recovered patients showing multiple or one-sided infiltrations (18). Goicoechea and Ma reported a ground glass radiological appearance with bilateral and peripheral patterns in 85.7% and 64% of patients, respectively (25,26).
In our study, comparison of clinical and laboratory parameters between discharged and deceased hemodialysis patients with COVID-19 demonstrated that non-survivors were generally older and exhibited elevated white blood cell counts and serum creatinine levels relative to recovered patients. Other laboratory values showed no significant differences between groups. Comorbidities such as diabetes were more common among the deceased patients, and their clinical presentation, including symptoms like weakness and lethargy, differed significantly from survivors (27). These findings are consistent with the research by Zhou et al. (2020), which reported higher mortality rates associated with comorbid conditions prevalent in hemodialysis patients, thus validating our results (28).
Laboratory analyses revealed that elevated white blood cell counts and serum creatinine levels were significant prognostic indicators associated with mortality. The absence of notable differences in other laboratory parameters underscores the need for further research to identify additional predictive biomarkers. In Valeri et al.’s study, a 14-day follow-up showed that 18 patients (31%) died within six days of hospital admission. Deceased patients had significantly higher baseline levels of white blood cells, lactate dehydrogenase (LDH), and C-reactive protein (CRP) compared to survivors (P-Value = 0.04) (18). Ma et al. involving 230 hemodialysis patients in Wuhan, China, 15 individuals (6.25%) died from COVID-19, with cardiovascular disease, cerebrovascular disease, and hyperkalemia identified as leading causes of death (29). Laboratory findings reveal that elevated WBC counts and creatinine levels serve as significant prognostic markers associated with mortality (19). Findings from Valeri's, Yiqiong et al.’s, and Fisher’s studies further support the adverse prognostic indicators identified in our research, including elevated inflammatory markers and underlying cardiovascular conditions.
This study showed a significant relationship between some demographic factors, comorbidities, symptoms, and laboratory findings with patient outcomes. For example, increased WBC count and creatinine level were identified as important prognostic markers associated with mortality. In addition, comorbidities such as diabetes were strongly associated with increased mortality rates. These findings emphasize the importance of comprehensive patient assessment and appropriate treatment strategies to optimize outcomes in this vulnerable population.
Despite the lack of long-term follow-up data, this study provides valuable insights into the acute effects of COVID-19 on hemodialysis patients. Future research should include long-term follow-up to assess ongoing outcomes and potential complications. Additionally, larger, multicenter studies are needed to validate these findings and explore further factors influencing outcomes in this vulnerable population. Enhanced preventive measures, early interventions, and regular monitoring using CT scans and laboratory markers are crucial for managing hemodialysis patients with COVID-19.
Conclusion
In summary, this study highlights the clinical outcomes of hemodialysis patients with COVID-19. While most patients were discharged, a notable mortality rate underscores the severity of the disease. Common symptoms and significant radiological findings emphasize the acute presentation of COVID-19 in this population. Laboratory markers, especially elevated WBC counts and creatinine levels, serve as important prognostic indicators. Management of comorbid conditions like diabetes is crucial, and the study underscores the need for vigilant monitoring and potentially more aggressive treatment strategies. Further research is warranted to validate these findings and explore additional factors affecting outcomes in hemodialysis patients with COVID-19.
Acknowledgement
The authors thank the research committee of Golestan University of Medical Sciences and also this work was supported by the research committee of Golestan University of Medical Sciences.
Funding sources
This work was supported by the Research Committee of Golestan University of Medical Sciences with the grant number IR.GOUMS.REC.1399.377.
Ethical statement
Ethical approval was obtained from the Golestan University research committee, under approval number IR.GOUMS.REC.1399.377. Written informed consent was obtained from all patients or their legal guardians before their inclusion in the study. All patient data were anonymized to ensure privacy and confidentiality.
Conflicts of interest
The authors have no financial or proprietary interests in any material discussed in this article.
Author contributions
The role of each participant is as follows: SA and MM conceived this study and were the supervisors. SJ, and AR. collected and analyzed the data. Also, ZM and AR. drafted the manuscript. All authors read and approved the final version of the manuscript.
Type of Article: Original article |
Subject:
General medicine
Received: 2023/07/21 | Accepted: 2024/04/30 | Published: 2024/12/28
Received: 2023/07/21 | Accepted: 2024/04/30 | Published: 2024/12/28
References
1. Husain SA, Dube G, Morris H, Fernandez H, Chang JH, Kathryn Paget K, et al. Early Outcomes of Outpatient Management of Kidney Transplant Recipients with Coronavirus Disease 2019. Clin J Am Soc Nephrol. 2020:15(8):1174-8. [View at Publisher] [DOI] [PMID] [Google Scholar]
2. Aziz F, Mandelbrot D, Singh T, Parajuli S, Garg N, Mohamed M, et al. Early Report on Published Outcomes in Kidney Transplant Recipients Compared to Nontransplant Patients Infected With Coronavirus Disease 2019. Transplant Proc. 2020;52(9):2659-62. [View at Publisher] [DOI] [PMID] [Google Scholar]
3. Ajaimy M, Melamed ML. COVID-19 in Patients with Kidney Disease. Clin J Am Soc Nephrol. 2020;15(8):1087-9. [View at Publisher] [DOI] [PMID] [Google Scholar]
4. Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507-13. [View at Publisher] [DOI] [PMID] [Google Scholar]
5. Lu R, Zhao X, Li J, Niu P, Yang B, Wu H, et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. 2020;395(10224):565-74. [View at Publisher] [DOI] [PMID] [Google Scholar]
6. Basile C, Combe C, Pizzarelli F, Covic A, Davenport A, Kanbay M, et al. Recommendations for the prevention, mitigation and containment of the emerging SARS-CoV-2 (COVID-19) pandemic in haemodialysis centres. Nephrol Dial Transplant. 2020;35(5):737-41. [View at Publisher] [DOI] [PMID] [Google Scholar]
7. Cheng Y, Luo R, Wang K, Zhang M, Wang Z, Dong L, et al. Kidney disease is associated with in-hospital death of patients with COVID-19. Kidney Int. 2020;97(5):829-38. [View at Publisher] [DOI] [PMID] [Google Scholar]
8. Yang X, Yu Y, Xu J, Shu H, Xia J, Liu H, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020;8(5):475-81. [View at Publisher] [DOI] [PMID] [Google Scholar]
9. Pan XW, Xu D, Zhang H, Zhou W, Wang LH, Cui XG. Identification of a potential mechanism of acute kidney injury during the COVID-19 outbreak: a study based on single-cell transcriptome analysis. Intensive Care Med. 2020;46(6):1114-6. [View at Publisher] [DOI] [PMID] [Google Scholar]
10. Kooman JP, Sande FM van der. COVID-19 in ESRD and Acute Kidney Injury. Blood Purif. 2021;50(4-5):610-20. [View at Publisher] [DOI] [PMID] [Google Scholar]
11. Mohamed MMB, Lukitsch I, Torres-Ortiz AE, Walker JB, Varghese V, Hernandez-Arroyo CF, et al. Acute Kidney Injury Associated with Coronavirus Disease 2019 in Urban New Orleans. Kidney360. 2020;1(7):614-22. [View at Publisher] [DOI] [PMID] [Google Scholar]
12. Sharma S, Aggarwal A, Sharma RK, Patras E, Singhal A. Correlation of chest CT severity score with clinical parameters in COVID-19 pulmonary disease in a tertiary care hospital in Delhi during the pandemic period. Egypt J Radiol Nucl Med. 2022;53(1):166. [View at Publisher] [DOI] [Google Scholar]
13. Ajaimy M, Melamed ML. COVID-19 in Patients with Kidney Disease. Clin J Am Soc Nephrol. 2020;15(8):1087-9. [View at Publisher] [DOI] [PMID] [Google Scholar]
14. Wu J, Li J, Zhu G, Zhang Y, Bi Z, Yu Y, et al. Clinical features of maintenance hemodialysis patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. Clin J Am Soc Nephrol. 2020;15(8):1139-45. [View at Publisher] [DOI] [PMID] [Google Scholar]
15. Grasselli G, Z A, Zanella A, Antonelli M, Cabrini L, Castelli A, et al. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy Region, Italy. JAMA. 2020;323(16):1574-81. [View at Publisher] [DOI] [PMID] [Google Scholar]
16. Madjid M, Safavi-Naeini P, Solomon SD, Vardeny O. Potential effects of coronaviruses on the cardiovascular system: a review. JAMA Cardiol. 2020;5(7):831-40. [View at Publisher] [DOI] [PMID] [Google Scholar]
17. Xiong F, Tang H, Liu L, Tu C, Tian JB, Lei CT, et al. Clinical Characteristics of and Medical Interventions for COVID-19 in Hemodialysis Patients in Wuhan, China. J Am Soc Nephrol. 2020;31(7):1387-97. [View at Publisher] [DOI] [PMID] [Google Scholar]
18. Valeri AM, Robbins-Juarez SY, Stevens JS, Ahn W, Rao MK, Radhakrishnan J, et al. Presentation and Outcomes of Patients with ESKD and COVID-19. J Am Soc Nephrol. 2020;31(7):1409-15. [View at Publisher] [DOI] [PMID] [Google Scholar]
19. Kroll MK, Schloer S, Candan P, Korthals N, Wenzel C, Ihle H, et al. Importance of ACE2 for SARS-CoV-2 Infection of Kidney Cells. Biomolecules. 2023;13(3):472. [View at Publisher] [DOI] [PMID] [Google Scholar]
20. Salazar E, Christensen PA, Graviss EA, Nguyen DT, Castillo B, Jian Chen J, et al. Treatment of Coronavirus Disease 2019 Patients with Convalescent Plasma Reveals a Signal of Significantly Decreased Mortality. Am J Pathol. 2020;190(11):2290-303. [View at Publisher] [DOI] [PMID] [Google Scholar]
21. Chai X, Hu L, Zhang Y, Han W, Lu Z, Ke A, et al. Specific ACE2 Expression in Cholangiocytes May Cause Liver Damage After 2019-nCoV Infection. bioRxiv. 2020. [View at Publisher] [DOI] [Google Scholar]
22. Fisher M, Yunes M, Mokrzycki MH, Golestaneh L, Alahiri E, Coco M. Chronic hemodialysis patients hospitalized with COVID-19-short-term outcomes in Bronx, New York. Kidney360. 2020;1(8):755-62. [View at Publisher] [DOI] [PMID] [Google Scholar]
23. Du X, Li H, Dong L, Li X, Tian M, Dong J. Clinical features of hemodialysis patients with COVID-19: a single-center retrospective study on 32 patients. Clin Exp Nephrol. 2020;24(9):829-35. [View at Publisher] [DOI] [PMID] [Google Scholar]
24. Adwan L, Al-Sadi T, Shawakha S, Al-Shami NA. Clinical outcomes of COVID-19 in hemodialysis patients. Front Med (Lausanne). 2023;10:1281594. [View at Publisher] [DOI] [PMID] [Google Scholar]
25. Goicoechea M, Cámara LAS, Macías N, Morales AM, Rojas ÁG, Bascuñana A, et al. COVID-19: clinical course and outcomes of 36 hemodialysis patients in Spain. Kidney Int. 2020;98(1):27-34. [View at Publisher] [DOI] [PMID] [Google Scholar]
26. Ma Y, Diao B, Lv X, Liang W, Zhu J, Liu L, et al. COVID-19 in hemodialysis (HD) patients: Report from one HD center in Wuhan, China. medRxiv. 2020. [View at Publisher] [DOI] [Google Scholar]
27. Zhou F, YT, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054-62. [View at Publisher] [DOI] [PMID] [Google Scholar]
28. Keller N, Chantrel F, Krummel T, Bazin-Kara D, Faller AL, Muller C, et al. Impact of first-wave COronaVIrus disease 2019 infection in patients on haemoDIALysis in Alsace: the observational COVIDIAL study. Nephrol Dial Transplant. 2020;35(8):1338-411. [View at Publisher] [DOI] [PMID] [Google Scholar]
29. Ma Y, Diao B, Lv X, Zhu J, Chen C, Liu L, et al. Epidemiological, clinical, and immunological features of a cluster of COVID-19-contracted hemodialysis patients. Kidney Int Rep. 2020;5(8):1333-41. [View at Publisher] [DOI] [PMID] [Google Scholar]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |